
There is no evidence that adequate nutritional support promotes accelerated tumor growth in humans. Therefore, calorie intake in cancer patients is recommended to be similar to that of healthy people. The recommended daily calorie intake is measured according to height, weight and physical activity and usually ranges between 25 to 30 kcal/kg/day.
It is very important to maintain a patient’s lean muscle mass during treatment. Patients with higher levels of lean muscle mass tolerate treatments better and reach better final results from their therapy. Therefore, there is a recommendation for increased protein intake between 1 and 1.5 g/kg/day, which should represent 20 to 35% of total daily energy intake. The recommended proportion of carbohydrates is 40 to 50% of total energy intake and the recommended fat proportion is 25 to 35%.
Older age, lack of physical activity and systemic inflammation due to antitumor treatment are known to induce anabolic resistance, i.e. reduced sensitivity of protein synthesis to anabolic stimuli.
Recommendations in older, chronically ill people are for increased protein intake of 1.0 to 1.5 g/kg/day as the amino acid and protein doses capable of maintaining a positive protein balance in older cachectic patients may reach up to 2 g/kg/day. In patients with chronic kidney disease the protein supply should not exceed 1.0 to 1.2 g/kg/day.
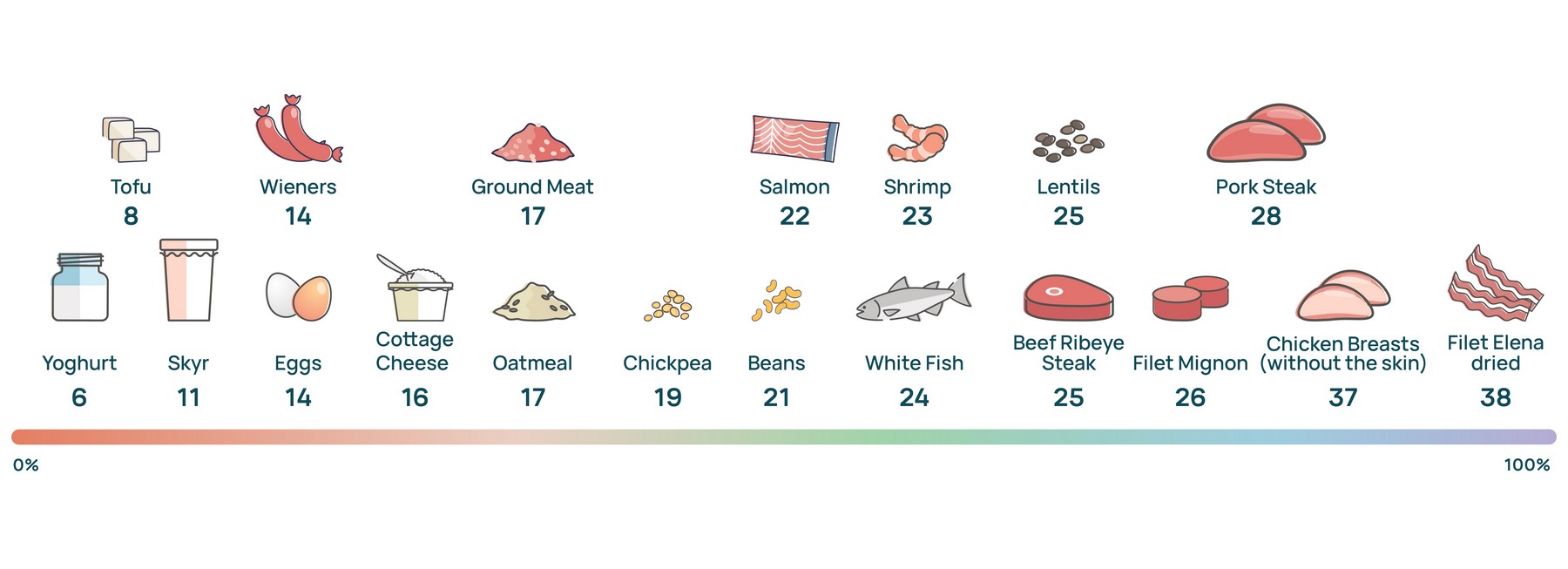
Many dietary strategies recommend different ways to increase protein intake, such as consuming the protein food first or adding protein powder to the meal to satisfy the body’s increased protein demands. Consumption of unprocessed foods with a high percentage of protein and calories such as eggs, fish, beef, chicken, turkey, seafood, legumes, cottage cheese, yogurt etc. is recommended. It is necessary to limit intake of dry and salted meats with a high percentage of saturated fatty acids such as dry cold meats, pork, sausages, bacon, meatballs, etc.
Amount of protein per 100g product
The recommended proportion of carbohydrates for cancer patients is 40 to 50% of total daily energy intake. There are many conflicting opinions regarding carbohydrate consumption in cancer patients. It is important to know that the main role of carbohydrates is to provide the energy necessary for the function of normal cells and tissues in the body. The typical energy demand of cancer cells is many times (sometimes up to 40 times) higher compared to normal tissue. It is important to understand that effective management, rather than restriction, of the body’s preferred fuel intake, carbohydrates, helps control the fuel available to cancer cells as well.
A good way to ensure smooth and stable levels of carbohydrate energy for the body’s demands and limit the energy available to cancer is by consuming mostly low glycemic index complex carbohydrates and limiting high glycemic index simple carbohydrates.
Low glycemic index foods contain plant fiber, polyphenols and saponins and other healthy nutrients that do not cause an insulin spike and provide the body with high amounts of vitamins and minerals. Such food products are: spinach, olives, cucumbers, brown and black rice, bulgur, quinoa, carrots, tomatoes, green beans, red lentils, mushrooms, zucchini, pumpkin seeds, asparagus, cabbage, raw nuts, whole grains of high fiber content, dark chocolate (containing more than 80% of cocoa), fresh low-sugar fruits such as blueberries, strawberries, blackberries, raspberries, apples, quince, pomegranate, etc.
High glycemic index foods contain high absorption rate simple carbohydrates that cause a serum glucose spike. Such food products are: white flour, white bread, sweets, jams, stewed fruits, honey, potatoes, granola, white rice, milk chocolate, pumpkin, white and brown sugar, high-sugar sweet fruits such as melon, watermelon, banana, pear, peach, etc.
The recommended fat proportion is 25 to 35% (in some cases up to 40%) of total daily macronutrient intake. Most fats are recommended to be obtained from nutritional sources that are rich in polyunsaturated (Omega-3 and 6) and monounsaturated (Omega-9) fatty acids in their natural form that have not been exposed to chemical or high-heat processing. Such sources of healthy fats are: most nuts (walnut, almond, macadamia, pecan, peanut, pumpkin seed, chia), olives, avocado, fish, algae oil, cold-pressed oils such as olive oil, rapeseed oil, etc.
Excessive and unbalanced consumption of foods high in saturated fatty acids such as palm and coconut oil, high-fat meat (pork, chicken skin) and other animal products such as cow butter, cheese and milk, except skimmed milk, should be limited (but not completely stopped). Intake of saturated fatty acids should be around 20 g/d.
Trans-fatty acids should NOT be consumed. Trans fats are entirely unhealthy because they cause strong inflammatory reactions in the body. The main source of industrially produced trans-fatty acids are partially hydrogenated oils, which are produced by high-heat and/or chemical processing of unsaturated vegetable oils. They are most commonly used in the food industry to produce a large number of semi-finished and packaged foods. They are present in large amounts in margarine, crisps and snacks, biscuits, wafers, cakes and other savory and sweet baked goods, frozen potatoes, frozen pizza and other dough.
Intake of marine-derived Omega-3 fatty acids EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) should be optimized.
The Western dietary pattern is largely associated with a disproportionate intake of saturated fatty acids, unsaturated fatty acids (Omega 3 ALA; Omega 6 and 9), trans fats and saturated fatty acids to Omega-3 EPA/DHA in the range of 20 to 30:1, which is associated with the pathogenesis of many diseases, including cardiovascular, oncological, inflammatory and autoimmune diseases.
The signaling molecules (intraleukins, prostaglandins, etc.) produced by the said fats are more powerful mediators of inflammation compared to marine-derived Omega-3 EPA/DHA fatty acids.
Advanced (stage IV) cancer patients undergoing chemotherapy and at risk of weight loss are recommended to take long-chain Omega-3 fatty acids (EPA and DHA) of 1 to 4 g a day to reduce inflammatory reactions, improve appetite, counteract malnutrition and preserve lean body mass and body weight.
A high intake of Omega-3 EPA and DHA may be ensured by consumption of herring, wild salmon, tuna, mackerel, sardines, anchovies, lake trout, supplementation with algae oil and fish oil in the form of a dietary supplement.
Plant-based Omega-3 fatty acids (ALA) have significantly lower helpful biological activity and cannot replace the healthy effects of marine-derived Omega-3 fatty acids (EPA and DHA).
IMPORTANT: In some more sensitive people intake of high doses exceeding 1 g/d of Omega-3 EPA and DHA fatty acids in the fasting state may cause a slight laxative effect. In this case temporarily reduce intake dose according to individual sensitivity.
In summary:
The optimal ratio of fatty acids should represent 25 to 35% of the body’s daily calorie demands in approximate indicative proportions of 8:4:1 of Omega-3 ALA, 6 and 9 unsaturated fatty acids to saturated fatty acids to Omega-3 EPA/DHA unsaturated fatty acids with zero or minimal trans fat intake.
An easy way to distinguish among the different types of fatty acids is that due to differences in their chemical structure at room temperature saturated fatty acids turn solid (butter, lard), while unsaturated fatty acids are in liquid form (olive oil, cooking oil, fish oil). Trans fats are often vegetable oils that have undergone prolonged high-heat and/or chemical processing. They are present in margarine, snacks and crisps.
It is important to avoid dehydration while undergoing antitumor treatment. Good hydration is important to reduce side effects of treatment such as nausea, weakness, headache, constipation and fatigue. Aim to take 6 to 8 glasses (2 to 3 liters) of water a day. Include more hydrating foods in your diet such as fruits, vegetables, soups, juices, etc. Limit caffeine and alcohol, which may dehydrate your body. Don’t wait until you are thirsty to drink water. Drink water consistently throughout the day. Carry a water bottle with you to remind you to hydrate on a regular basis.
Fasting during treatment with chemotherapy agents is not recommended as it carries a risk of developing malnutrition if not done properly. Some of the most common side effects of these therapies are loss of appetite, nausea and vomiting. Practicing fasting in the presence of the said toxicities may exacerbate malnutrition and potentiate additional weight loss. Small but frequent meals spread evenly throughout the day as well as intake of antiemetics, antacids and other drugs to counteract the side effects of chemotherapy are recommended.