
Chronic noncommunicable diseases (CNCDs) are the number one cause of death and disability in developed countries. These diseases kill 41 million people every year and are responsible for 71% of all deaths worldwide.
Chronic noncommunicable diseases refer to a group of conditions that are not primarily caused by an acute infection or injury, lead to long-term health consequences and often create the need for long-term treatment and care. These conditions include cancer, cardiovascular diseases, diabetes and chronic lung diseases, autoimmune diseases, etc.
Many chronic noncommunicable diseases can be prevented by eliminating common risk factors such as tobacco use, excessive alcohol use, lack of physical activity and unhealthy diet.
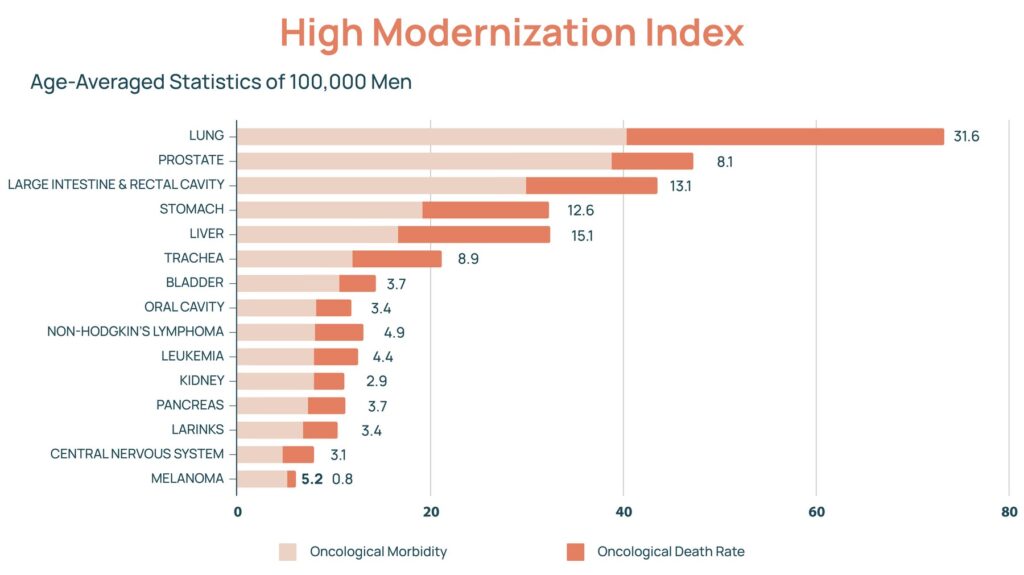
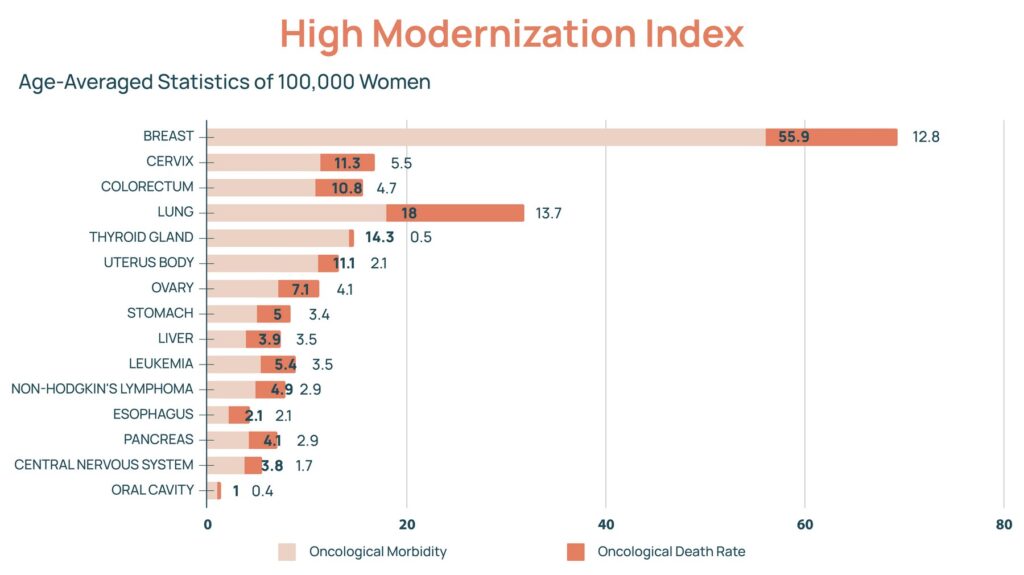
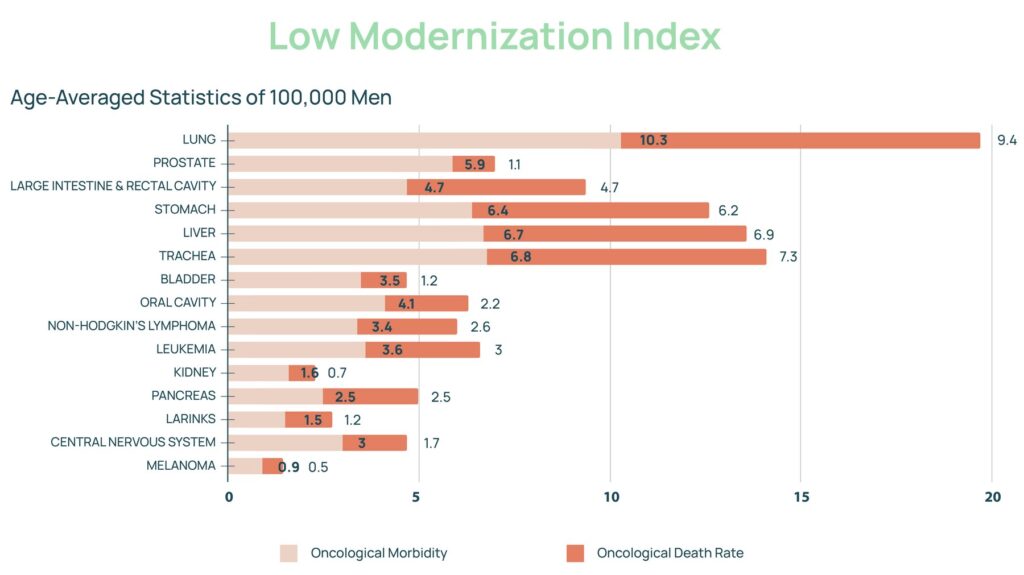
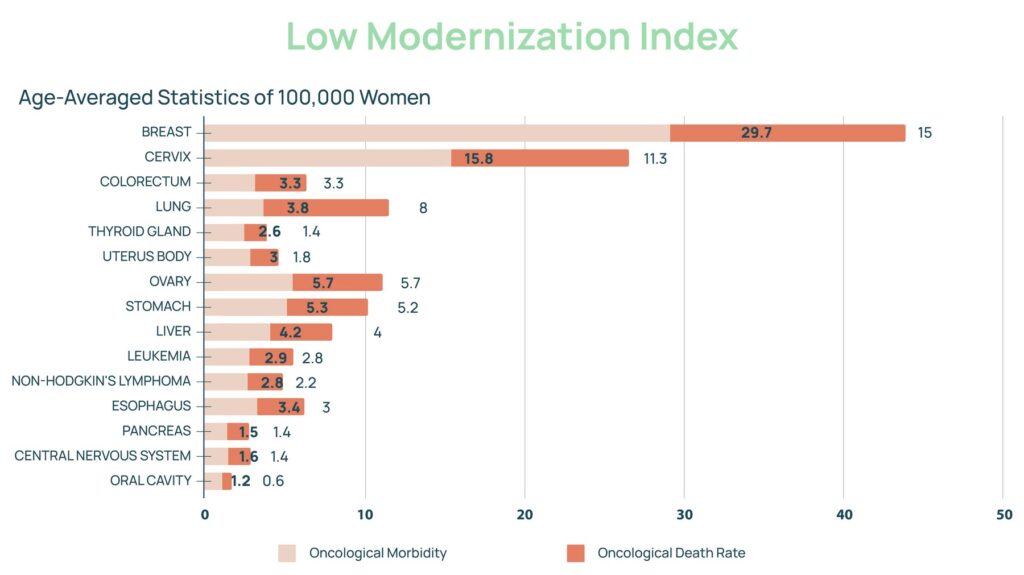
The increased Human Development Index (HDI) is directly related to CNCD incidence. Among all chronic noncommunicable diseases, newly diagnosed cancers have the strongest correlation with the Human Development Index. The chart below illustrates the difference between the incidence and mortality of different cancers between countries with high and low Development Index.
Hectic and at the same time sedentary lifestyle of modern times, mental and emotional distress, lack of healthy dietary and physical culture, polluted environment and difficulty in accessing quality food products have determined the statistical boom of cancer diseases in the 21st century, highly dependent on both genetic and external factors.
Paradoxically, however, not all high HDI countries have the same cancer incidence. The explanation is reduced to several key differences in everyday living, culture and lifestyle of the inhabitants of these countries:
Comparing the statistics of the countries with the highest number of diagnosed cancers per 100,000 people, we see that Christian countries with developed healthcare systems, a Western dietary pattern and no strong religious lifestyle prevail. Australia (452), New Zealand (422), Ireland (372), the United States (362), Denmark (351), etc. top this ranking.
Looking at the statistics for the countries with the lowest number of diagnosed cancers per 100,000 people, we see that Muslim countries with moderately well-developed healthcare systems, an Eastern Mediterranean dietary pattern, a strict religious lifestyle (observing religious fasting, avoiding certain foods) prevail.
Representatives of such countries are Saudi Arabia (96), Yemen (97), Oman (103), the United Arab Emirates (106), Qatar (107).
A direct comparison between Australia (452 cases per 100,000) and the United Arab Emirates (106 cases per 100,000), two high HDI countries, shows a more than fourfold difference in cancer incidence between the two countries due largely to:
Researchgate statistics demonstrate a significant difference in the knowledge and habits of an average member of the said countries for the use of foods, herbs and extracts both in daily cooking activities and as alternative traditional medicine for the treatment of various trivial pathological conditions such as acne, cough, constipation and headache in favor of the United Arab Emirates.
Significant difference in daily alcohol use
Statistics show that the average annual alcohol use in the United Arab Emirates is about 3.85 liters of hard alcohol per capita, while in Australia it is 10.36 liters.
Difference in healthy eating habits
High consumption of processed foods, salt and sugar and low consumption of fish, whole grains, legumes, fruits, vegetables and nuts in daily life are associated with both increased risk of cardiovascular and metabolic diseases and increased cancer incidence. Global Nutrition Report statistics show a nearly threefold difference in annual cancer mortality associated with unhealthy eating habits in these countries (about 14,000 for Australia and 5,000 for the UAE per every 1 million people). In addition, reduced consumption of some of the more unhealthy foods such as pork red meat is reported in the UAE as part of their culture and religion.
Fasting
In Muslim countries over 90% of the population practices mandatory religious fasting (Ramadan), which is practiced for 1 month every year and is a 14-hour abstinence from food and water during daylight hours. Such abstinence is known as moderate fasting in Western countries. Moderate fasting has a number of health benefits, including weight regulation, improved blood sugar levels, reduction of inflammatory processes in the body, improved heart health and reduction of cancer risk.
The health effects of moderate fasting are thought to result from the induction of cell autophagy processes. Autophagy is an important process required to maintain proper cellular homeostasis. It is responsible for the disposal and recycling of metabolic macromolecules and damaged cell organelles by inducing cellular lysosomal degradation processes. Under stressful conditions, including nutrient deficiency, autophagy is significantly activated to ensure maintenance of proper cell function and survival of healthy cells.
Conclusion
There are obvious differences in the daily lifestyle of the average members of these territories, including healthy eating habits, such as increased intake of fruits, vegetables, nuts, herbs, fish and seafood and reduced intake of trans fats, red meat, processed meat products and alcohol. There are also huge statistical differences in the percentage of the population observing some form of diet, eating and fasting regimen or religious fasting.
Taking also into account the fact that the lower cancer incidence in the UAE is in the presence of additional negative factors, such as lower average physical activity, higher smoking rate, higher obesity rate, lower healthcare budget, similar average age and higher index of polluted environment, the importance of healthy food, low alcohol use and good dietary culture is further emphasized as one of the main preventive measures against development of both cancer and other chronic noncommunicable diseases